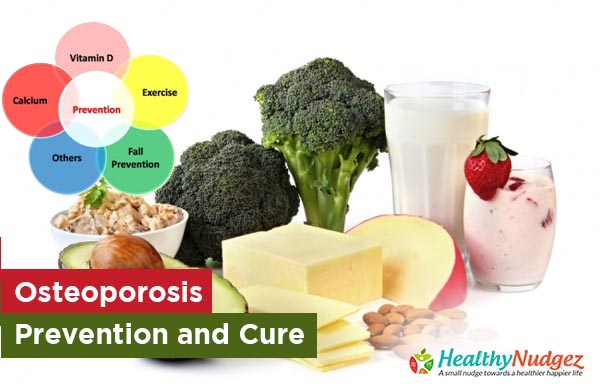
Osteoporosis- Prevention and Cure
Osteoporosis is a disease of the skeletal system characterized by low bone mass and structural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture.
More than 200 million women worldwide have osteoporosis. Literature suggests that osteoporosis is not uncommon in India and there are around 50 million osteoporotic women in India. Secondly, osteoporotic fractures (especially of the hip) occur more frequently in Indian males than females. And thirdly osteoporotic fractures usually occur 10 – 20 years earlier in Indian men and women as compared to Caucasian population. Recent data indicates a high prevalence of vitamin D deficiency in urban Indians despite availability of sunshine.
Bone strength reflects the integration of 2 main factors: Bone quality and Bone mineral density or bone mass.
Osteoporosis may be primary or secondary. Primary Osteoporosis is age related or post-menopausal. Secondary Osteoporosis may be due to endocrine diseases like Cushing’s syndrome, Hyperthyroidism and Hypogonadism in males, GI disorders like IBD (irritable bowel disease) and malabsorption syndrome, Drugs like corticosteroids, cancer chemotherapy, phenytoin, heparin, barbiturates, aluminum containing antacids, Multiple myeloma, CRF, Prolonged immobilization and Inflammatory arthritis like RA or AS.
Risk factors for Osteoporosis:
Personal characteristics
- Age >55
- BMI < 19
- Abnormal menstrual history – late menarche, long term menstrual irregularities, early menopause (<45 yrs) (natural or surgical)
- Family h/o osteoporotic fractures
- Past h/o fragility fractures
- H/o eating disorder / strict dieting
Lifestyle factors
- Smoking
- Alcoholism
- Inactive lifestyle (low physical activity)
- Low calcium intake
- Little sun exposure
- Consumption of large amounts of caffeine
Diagnosis of Osteoporosis
In absence of any reliable methods of measuring bone quality, the diagnosis of osteoporosis is currently based on the determination of bone mineral density (BMD) by bone densitometry. It is most useful in identifying patients who have secondary causes of osteoporosis.
Patients should be subjected to BMD measurement only if, there are strong clinical risk factors or for monitoring patients on treatment.
Contraindications for densitometry include pregnancy, recent G.I. contrast studies and radionuclide tests (wait for at least 7 days).
BMD should not be repeated if an optimal level is achieved).
Management of Osteoporosis.
Goals of therapy in the management of osteoporosis are –
- Prevention of fractures
- Optimization of skeletal development and maximization of bone mass
- Prevention of age related and secondary causes of bone loss
- Preservation of structural integrity of the skeleton
- Improvement in quality of life
- Decrease in morbidity and mortality
Since no therapy fully restores lost bone mass, the importance of prevention can never be understated. Ideally the message to invest in bone health should begin from menarche since peak bone mass is achieved by late twenties. Public education should be made a priority issue. Only when the common man is convinced about the problem and the need to prevent it, especially when it is preventable, will he or she be sufficiently motivated to prevent osteoporosis.
Individual based strategies are divided into non-pharmacological and pharmacological management. In the former, lifestyle modification forms the cornerstone for prevention of osteoporosis. This includes physical exercise, which improves bone strength, muscular performance, joint flexibility, balance, functional capacity and reduces incidences of falls, dietary habits which should include foods rich in calcium and vitamin D and avoiding excessive caffeine intake (which increases calcium excretion and is associated with modest increase in fracture risk) and quitting alcohol intake and smoking.
Pharmacological management of osteoporosis includes the use of -
- Calcium and Vitamin D supplements
- Bisphosphonates
- Selective estrogen receptor modulator (SERM)
- Calcitonin
- Anabolic agents
- Strontium Ranelate
Calcium and Vitamin D supplements are to be used only if dietary intake of calcium and production of vitamin d is less. They have shown to increase BMD and reduce fracture rates. Exceeding the recommended daily calcium intake offers no health benefit and may be harmful. Calcium decreases the absorption of iron, tetracyclines and quinolones. Side effects include constipation, bloating, cramps and flatulence. Estimated daily requirement of Vitamin D is around 400 I.U. but varies through different stages of life. Older patients with severe osteoporosis need 800 to 1000 I.U. per day. 25 minutes of sunlight on the face and the forearms is usually sufficient for the body to generate adequate amounts of vitamin D. Safe upper limit of vitamin D intake is 2000 I.U/ day. Higher doses may cause hypercalciuria and hypercalcaemia.
Bisphosponates are potent inhibitors of bone resorption (breakdown of bone tissues and release of bone minerals into blood) and therefore slow down bone loss and reduce risk of fractures.
Selective Estrogen Receptor Modulator (SERM) has mixed effects on estrogen receptors. Raloxifene has estrogen like effects on lipid metabolism and bone. It significantly increases BMD and reduces risk of new and recurrent vertebral fractures in post-menopausal women. The risks are an increase in risk of venous thromboembolism up to three-fold and is therefore contra-indicated in women with a h/o thrombosis and increases leg cramps and hot flushes.
Calcitonin is a polypeptide hormone derived from Salmon. Calcitonin reduces outflow of calcium from bone to blood (bone resorption). It has shown to increase spine BMD in post-menopausal and decreases the risk of new vertebral fractures. Adverse effects include hypersensitivity reactions, flushing and nausea and skin rash.
Teriparatide is human parathyroid hormone. Skeletal effects of PTH differ according to pattern of systematic exposure – Continuous exposure leads to increased differentiation of osteoclasts (bone cells responsible for breakdown, repair and remodeling of bones) and increased bone resorption (as in hyperparathyroidism), but intermittent exposure of PTH preferentially stimulates osteoblasts (cells that synthesize bones) and thereby new bone formation. It is not administered to any patient with an increased baseline risk for developing osteosarcoma. PTH is also not recommended in patients with a history of Fypercalcaemia or hyperparathyroidism. Usual side effects include transient hypercalcaemia, dizziness and leg cramps.
Strotium ranelate increases bone formation in bone tissue, as well as osteoblasts and collagen synthesis. It reduces bone resorption by decreasing osteoclast differentiation. It has shown to reduce relative risk of new vertebral fractures. It is not recommended in children and adolescents, pregnant and lactating women and in patients with renal impairment. (No dose adjustment is required in hepatic impairment since strontium ranelate is not metabolized). Adverse effects include nausea, headache, diarrhoea, dermatitis and eczema.
Physical medicine and rehabilitation can reduce disability, improve physical function and lower the risk of subsequent falls in patients with osteoporosis. Rehabilitation and exercise are recognized means to improve function, such as activities of daily living. Psychosocial factors also strongly affect functional ability of the osteoporotic patient.