Sickle Cell Anaemia or Sickle cell disease
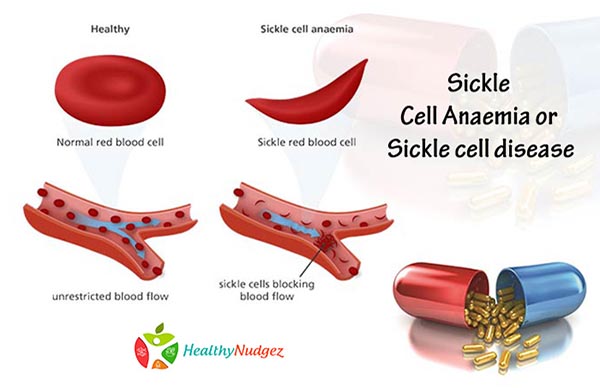
Sickle cell anaemia or Sickle cell disease is a genetic disorder, in which the body produces abnormally shaped red blood cells that have a crescent or sickle shape. These cells do not last as long as the normal, round red blood cells do (haemolysis), which leads to anaemia. Children with sickle cell anaemia show growth failure when compared to their healthy peers. This is due to anaemia, metabolic dysfunction and nutritional status.
Sickle cell disease(SCD) is most prevalent in Middle east, Southeast Asia, and sub-Saharan Africa especially Nigeria. About 5-7% of the world’s population has an abnormal haemoglobin gene. Africa and Asia are believed to be birthplace of SCD, which happened due to the natural mutation of the haemoglobin gene.
Apart from growth retardation, under-nutrition and anaemia, there are other symptoms associated with this disease, these are recurrent infections, abnormality of the spleen, chest pain, elevated white blood cell count, osteomyelitis (bone infection), osteoporosis, neurological abnormalities, abnormality of the blood vessels, elevated serum creatinine levels, low blood oxygen levels, lethargy, enlarged heat, gall stones, enlarged liver, blood in urine, jaundice, renal disease and many more.
SCD was first described in 1910, and efforts are being made since then to improve clinical care, to reduce the severity of symptoms, to lessen the frequency of hospitalization and decrease the recurrent painful episodes. However, only since the late 1980’s did undernutrition is being considered a serious complication of the disease that needs to be treated as a part of the required clinical care.
Nutritional deficiencies and Nutritional care of SCD
Studies have shown that body weight and BMI are directly related to the total haemoglobin levels, and also on the severity of SCD. This was also associated with inadequate nutrient intake resulting in frequent hospitalisation and overall growth retardation. This is due to increased demands and inadequate food intake. There is increased requirements of energy and protein due to the fact that these children have a higher basal metabolic rate (BMR) and increased resting energy expenditure, as compared to children their age group. Therefore, the Recommended Dietary Allowances for normal population are not sufficient for children with SCD.
The nutrients and foods of importance are as follows:
- Calories for improved metabolism, from all sources such as cereals, fruits, vegetables and fats in form of butter, oil etc.
- Protein foods such as milk, fish, poultry and meat, to improve lean body mass which has a positive effect on reducing complications associated with SCD
- Improved iron intake was associated with improve haemoglobin levels, reduced hemolysis and appear to be protective in SCD. Sources include all non-vegetarian sources, lentils, beans, etc.
- Calcium and phosphorus intakes are inversely related to frequency of hospitalisations found mostly in milk and milk products along with poultry.
- Vitamins D and E and folic acid are of importance especially during adolescence to improve growth
- Vitamin B group is also significantly related inversely to haemoglobin levels.
- Keep a good hydration, take lots of liquids such as soups, coconut water, lemon water, chaach etc, also individuals with sickle cell anemia should consume at least 8-10 glasses of water daily, according to the NHLBI.
- The UIHC recommends five to nine servings of fresh fruits and vegetables daily for individuals with sickle cell anemia.
- Fruits and vegetables such as berries, citrus fruits, watermelon, musk melon and green leafy vegetables are great sources of essential vitamins, minerals, antioxidants and dietary fiber.
Current SCD treatment guidelines only underline the importance of specific micronutrients, such as folic acid zinc and iron for their contribution in reducing inflammation and improving immunity, but along with and adequate overall nutritional intake. This is however, very clear from studies, that a targeted nutritional intervention can reduce the clinical severity of the disease. Nutritional Supplementation may also be required for these children on a regular basis.